Developing a dental checkup routine helps children understand the importance to keeping teeth healthy. It also helps children familiarize the dental environment.
At Smilerite, we want your child's dental visit to be as comfortable and enjoyable as possible. Getting to know the dentist and staff helps the child build trust and feel at ease for future dental visits.
At our office, we take extra care in painless dentistry for not only adults but also in young patients. We use dental care techniques to calm young children. With adequate pain control, you will be surprised how the children will let us do whatever is necessary.


Our young patients can watch a movie or listen to music during the dental procedure to block the unpleasant noise. This can help the child minimize the fear.
Fluoride Treatment
Fluoride is the most effective agent available to help prevent tooth decay. It is a mineral that is naturally present in varying amounts in almost all foods and water supplies. The benefits of fluoride have been well known for over 50 years and are supported by many health and professional organizations.
Fluoride works in two ways:
1. Topical fluoride
Topical fluoride strengthens the teeth once they have erupted by seeping into the outer surface of the tooth enamel, making the teeth more resistant to decay. We gain topical fluoride by using fluoride containing dental products such as toothpaste, mouth rinses, and gels. Dentists and dental hygienists generally recommend that children have a professional application of fluoride twice a year during dental check-ups.
2. Systemic fluoride
Systemic fluoride strengthens the teeth that have erupted as well as those that are developing under the gums. We gain systemic fluoride from most foods and our community water supplies. Generally, fluoride drops are recommended for infants, and tablets are suited for children up through the teen years. If too much fluoride is consumed while the teeth are developing, a condition called fluorosis (white spots on the teeth) may result.
Although most people receive fluoride from food and water, sometimes it is not enough to help prevent decay. Your dentist or dental hygienist may recommend the use of home and/or professional fluoride treatments for the following reasons:
-
Deep pits and fissures on the chewing surfaces of teeth
-
Exposed and sensitive root surfaces
-
Fair to poor oral hygiene habits
-
Frequent sugar and carbohydrate intake
-
Inadequate exposure to fluorides
-
Inadequate saliva flow due to medical conditions, medical treatments or medications
-
Recent history of dental decay
Remember, fluoride alone will not prevent tooth decay! It is important to brush at least twice a day, floss regularly, eat balanced meals, reduce sugary snacks, and visit your dentist on a regular basis.






Sealants
A sealant is a thin, plastic coating applied to the chewing surface of molars, premolars and any deep grooves (called pits and fissures) of teeth. More than 75% of dental decay begins in these deep grooves. Teeth with these conditions are hard to clean and are very susceptible to decay. A sealant protects the tooth by sealing deep grooves, creating a smooth, easy to clean surface.
- Children and teenagers– As soon as the six-year molars (the first permanent back teeth) appear or any time throughout the cavity prone years of 6-16.
- Adults– Tooth surfaces without decay that have deep grooves or depressions.
- Baby teeth– Occasionally done if teeth have deep grooves or depressions and child is cavity prone.
Sealants are easily applied by your dentist or dental hygienist and the process takes only a couple of minutes per tooth.
The teeth to be sealed are thoroughly cleaned and then surrounded with cotton to keep the area dry. A special solution is applied to the enamel surface to help the sealant bond to the teeth. The teeth are then rinsed and dried. Sealant material is carefully painted onto the enamel surface to cover the deep grooves or depressions. Depending on the type of sealant used, the material will either harden automatically or with a special curing light.
Proper home care, a balanced diet, and regular dental visits will aid in the life of your new sealants.
Pulp Therapy


The “pulp” of a tooth cannot be seen with the naked eye. Pulp is found at the center of each tooth, and is comprised of nerves, tissue, and many blood vessels, which work to channel vital nutrients and oxygen. There are several ways in which pulp can be damaged. Most commonly in children, tooth decay or traumatic injury leads to painful pulp exposure and inflammation.
Pediatric pulp therapy is known by several other names, including: root canal, pulpotomy, pulpectomy, and nerve treatment. The primary goal of pulp therapy is to treat, restore, and save the affected tooth.
Dentists perform pulp therapy on both primary (baby) teeth and permanent teeth. Though primary teeth are eventually shed, they are needed for speech production, proper chewing, and to guide the proper alignment and spacing of permanent teeth.
What are the signs of pulp injury and infection?
Inflamed or injured pulp is exceptionally painful. Even if the source of the pain isn’t visible, it will quickly become obvious that the child needs to see the pediatric dentist.
Here are some of the other signs to look for:
- Constant unexplained pain.
- Nighttime pain.
- Sensitivity to warm and cool food temperatures.
- Swelling or redness around the affected tooth.
- Unexpected looseness or mobility of the affected tooth.
When should a child undergo pulp therapy?
Every situation is unique. The dentist assesses the age of the child, the positioning of the tooth, and the general health of the child before making a recommendation to extract the tooth or to save it via pulp therapy.
Some of the undesirable consequences of prematurely extracted/missing teeth are listed below:
- Arch length may shorten.
- In the case of primary tooth loss, permanent teeth may lack sufficient space to emerge.
- Opposing teeth may grow in a protruding or undesirable way.
- Premolars may become painfully impacted.
- Remaining teeth may “move” to fill the gap.
- The tongue may posture abnormally.
How is pulp therapy performed?
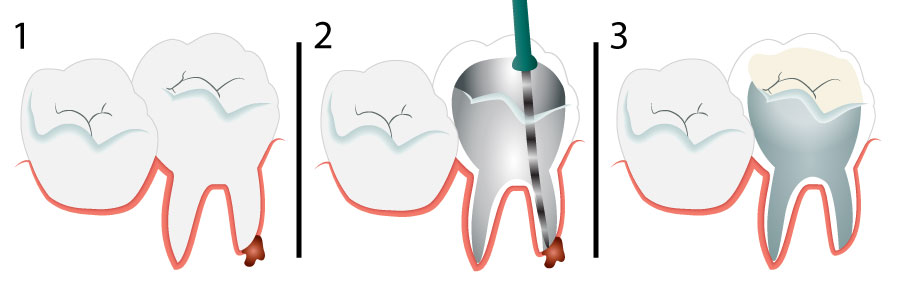
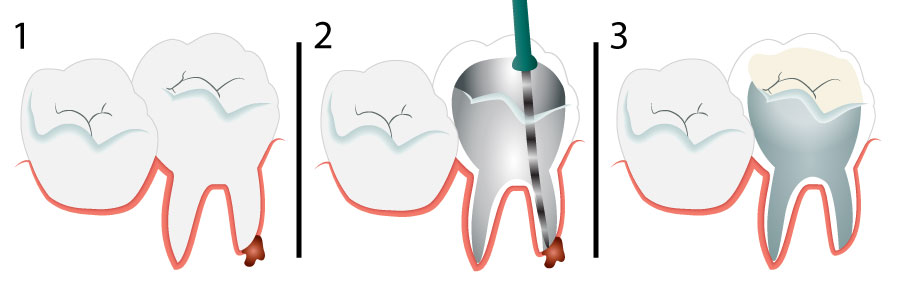
Initially, the dentist will perform visual examinations and evaluate X-rays of the affected areas. The amount and location of pulp damage dictate the nature of the treatment. Although there are several other treatments available, the pediatric pulpotomy and pulpectomy procedures are among the most commonly performed.
Pulpotomy - If the pulp root remains unaffected by injury or decay, meaning that the problem is isolated in the pulp tip, the dentist may leave the healthy part alone and only remove the affected pulp and surrounding tooth decay. The resulting gap is then filled with a biocompatible, therapeutic material, which prevents infection and soothes the pulp root. Most commonly, a crown is placed on the tooth after treatment. The crown strengthens the tooth structure, minimizing the risk of future fractures.
Pulpotomy treatment is extremely versatile. It can be performed as a standalone treatment on baby teeth and growing permanent teeth, or as the initial step in a full root canal treatment.
Pulpectomy - In the case of severe tooth decay or trauma, the entire tooth pulp (including the root canals) may be affected. In these circumstances, the dentist must remove the pulp, cleanse the root canals, and then pack the area with biocompatible material. This usually takes several office visits.
In general, reabsorbable material is used to fill primary teeth, and non-reabsorbable material is used to fill permanent teeth. Either way, the final treatment step is to place a crown on the tooth to add strength and provide structural support. The crown can be a natural-colored covering or stainless steel.
What are the signs of pulp injury and infection?
Inflamed or injured pulp is exceptionally painful. Even if the source of the pain isn’t visible, it will quickly become obvious that the child needs to see the pediatric dentist.
Here are some of the other signs to look for:
- Constant unexplained pain.
- Nighttime pain.
- Sensitivity to warm and cool food temperatures.
- Swelling or redness around the affected tooth.
- Unexpected looseness or mobility of the affected tooth.
When should a child undergo pulp therapy?
Every situation is unique. The dentist assesses the age of the child, the positioning of the tooth, and the general health of the child before making a recommendation to extract the tooth or to save it via pulp therapy.
Some of the undesirable consequences of prematurely extracted/missing teeth are listed below:
- Arch length may shorten.
- In the case of primary tooth loss, permanent teeth may lack sufficient space to emerge.
- Opposing teeth may grow in a protruding or undesirable way.
- Premolars may become painfully impacted.
- Remaining teeth may “move” to fill the gap.
- The tongue may posture abnormally.
How is pulp therapy performed?
Initially, the dentist will perform visual examinations and evaluate X-rays of the affected areas. The amount and location of pulp damage dictate the nature of the treatment. Although there are several other treatments available, the pediatric pulpotomy and pulpectomy procedures are among the most commonly performed.
Pulpotomy - If the pulp root remains unaffected by injury or decay, meaning that the problem is isolated in the pulp tip, the dentist may leave the healthy part alone and only remove the affected pulp and surrounding tooth decay. The resulting gap is then filled with a biocompatible, therapeutic material, which prevents infection and soothes the pulp root. Most commonly, a crown is placed on the tooth after treatment. The crown strengthens the tooth structure, minimizing the risk of future fractures.
Pulpotomy treatment is extremely versatile. It can be performed as a standalone treatment on baby teeth and growing permanent teeth, or as the initial step in a full root canal treatment.
Pulpectomy - In the case of severe tooth decay or trauma, the entire tooth pulp (including the root canals) may be affected. In these circumstances, the dentist must remove the pulp, cleanse the root canals, and then pack the area with biocompatible material. This usually takes several office visits.
In general, reabsorbable material is used to fill primary teeth, and non-reabsorbable material is used to fill permanent teeth. Either way, the final treatment step is to place a crown on the tooth to add strength and provide structural support. The crown can be a natural-colored covering or stainless steel.
HABIT BREAKING APPLIANCE
Thumb sucking can be a harder habit to break and tends to persist for longer without intervention. Children who continue to suck thumbs or pacifiers after the age of five (and particularly those who continue after permanent teeth begin to emerge) are at high-risk for developing dental complications.
How can thumb sucking and pacifier use damage children’s teeth?
Jaw misalignment – Pacifiers come in a wide range of shapes and sizes, most of which are completely unnatural for the mouth to hold. Over time, pacifiers and thumbs can guide the developing jaws out of correct alignment.
Tooth decay – Many parents attempt to soothe infants by dipping pacifiers in honey, or some other sugary substance. Oral bacteria feed on sugar and emit harmful acids. The acids attack tooth enamel and can lead to pediatric tooth decay and childhood caries.
Roof narrowing – The structures in the mouth are extremely pliable during childhood. Prolonged, repeated exposure to thumb and pacifier sucking actually cause the roof of the mouth to narrow (as if molding around the sucking device). This can cause later problems with developing teeth.
Slanting teeth – Growing teeth can be caused to slant or protrude by thumb and pacifier sucking, leading to poor esthetic results. In addition, thumb sucking and pacifier use in later childhood increase the need for extensive orthodontic treatments.
Mouth sores – Passive sucking is much less harmful than aggressive sucking. Aggressive sucking (popping sounds when the child sucks) may cause sores or ulcers to develop.
When can my child begin early orthodontic treatment?
Early orthodontic treatment aims to guide and regulate the width of both dental arches. The main goal of early treatment is to provide enough space for the permanent teeth to erupt correctly. Good candidates for early treatment include: children who have difficulty biting properly, children who lose baby teeth early, children whose jaws click or grind during movement, bruxers, and children who use the mouth (as opposed to the nose AND mouth) to breathe.
The goals of middle dentition treatments are to realign wayward jaws, to start to correct crossbites, and to begin the process of gently straightening misaligned permanent teeth. Middle dentition marks a developmental period when the soft and hard tissues are extremely pliable. In some ways therefore, it marks an optimal time to begin to correct a severe malocclusion.
Some appliances (like braces) are fixed and others are removable. Regardless of the appliance, the child will still be able to speak, eat, and chew in a normal fashion. However, children who are fitted with fixed dental appliances should take extra care to clean the entire oral region each day in order to reduce the risk of staining, decay, and later cosmetic damage.
Adolescent dentition is what springs to most parents’ minds when they think of orthodontic treatment. Some of the main goals of adolescent dentition include straightening the permanent teeth, and improving the esthetic appearance of the smile.
Most commonly during this period, the orthodontist will provide fixed or removable “braces” to gradually straighten the teeth. Upon completion of the orthodontic treatment, the adolescent may be required to wear a retainer in order to prevent the regression of the teeth to their original alignment.
Sports guard or Mouth guards
Protect Your Teeth during Sports Activities with a Mouth guard
Custom designed mouth guards are made of flexible plastic and molded to fit the shape of your teeth and therefore more comfortable than the readymade ones.
Mouth guards are recommended to protect your teeth, gums and jaw during sports activities, such as hockey, rugby, baseball and basketball, football, soccer or any other activity where your mouth may get hit.
-
Preventive Dentistry
-
Comfort Dentistry
-
Dental Care for Children
-
Restorative Dentistry
-
Cosmetic Dentistry
-
Endodontics
-
Oral Surgery
-
Dental Implants
-
Prosthodontics
-
Orthodontics