Extractions
A dental extraction is the removal of a tooth. There are a couple reasons why extractions might be needed. Extractions are performed for a wide variety of reasons, including tooth decay that has destroyed enough tooth structure to render the tooth non-restorable.
Wisdom Teeth Extractions
Third molars, commonly referred to as wisdom teeth, are usually the last four of 32 teeth to erupt (surface) in the mouth, generally making their appearance between the ages of 17 to 25. They are located at the back of the mouth (top and bottom), near the entrance to the throat. The term “wisdom” stems from the idea that the molars surface at a time typically associated with increased maturity or “wisdom”.


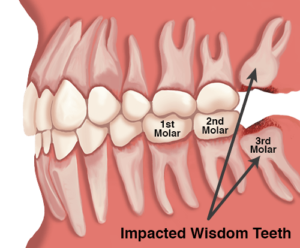
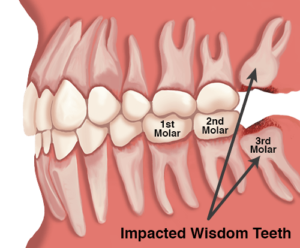
There are several types, or degrees, of impaction based on the actual depth of the teeth within the jaw:
Soft Tissue Impaction
The upper portion of the tooth (the crown) has penetrated through the bone, but the gingiva (gum) is covering part or all of the tooth’s crown and has not positioned properly around the tooth.
Partial Bony Impaction
The tooth has partially erupted, but a portion of the crown remains submerged below the gum and surrounding jawbone.
Complete Bony Impaction
The tooth is completely encased by jawbone. This will require more complex removal techniques.
Reasons to remove wisdom teeth
While not all wisdom teeth require removal, wisdom teeth extractions are most often performed because of an active problem such as pain, swelling, decay or infection, or as a preventative measure to avoid serious problems in the future. If impaction of one or more wisdom teeth is present, and left untreated, a number of potentially harmful outcomes can occur, including:
-
Damage to nearby teeth
-
Disease
-
Infection
-
Tooth Crowding
Exposure of Impacted Canine


Once the canine is exposed a small bracket is glued to the tooth. Attached to this is a chain which your orthodontist can then use to pull the tooth into the right position. The chain is usually stitched out of the way but it is quite delicate and therefore it is important to be careful when eating for the first few weeks after surgery.
Frenectomy


When frenum is attached high or between two upper front teeth, early removal can improve space closure of the front teeth. There is very little post-operative pain and swelling, and the patient can have normal function of the lips and tongue. Many patients hardly notice the effects of the surgery.
Apicoectomy
The teeth are held firmly in place by strong roots that extend into the jawbone. Molars and premolars tend to have several roots, whereas the front incisors only have a single root. The end or tip of each root is termed the apex. The apex is where the nerves and blood vessels enter the tooth, and aids in the delivery of blood to the crown (the part of the tooth you can see in your mouth).
A root canal treatment refers to the cleaning of the canals and the removal of infected and inflamed tissue within the root. When the inflammation or infection persists after the root canal treatment, an apicoectomy may be required. An apicoectomy is essentially the removal of the apex (or root tip), followed by a filling procedure to seal the root from further infection. When left untreated, infected roots can damage other teeth, spread infection, and cause regression of the jawbone.


Reasons for an apicoectomy
Infected and inflamed soft tissue around the root of a tooth can be exceptionally painful and debilitating to the patient. The purpose of an apicoectomy is to eliminate the infection in the tissue and to ultimately preserve the function of the tooth and save it from extraction. An apicoectomy will rarely be considered by the dentist unless a prior root canal treatment has failed.
There are several reasons why an apicoectomy may be necessary:
Small Adjoining Root Branches – Roots are extremely complex and can contain many tiny branches. If these tiny branches cannot be cleaned and sealed when the root canal treatment is performed, inflammation can persist.
Blocked Root Canal – In some cases, the dentist is unable to effectively clean a root canal because it is blocked by a fractured file left behind from prior root canal treatment. Infection and debris can quickly affect adjacent teeth.
Narrow or Curved Root Canals – When the root canal is poorly shaped, the endodontic files cannot reach the root tip. Continuing infection or re-infection can then occur.
What does getting an apicoectomy involve?
Prior to the surgery, the dentist will generally prescribe an antibiotic or anti-inflammatory medication to treat the underlying infection. Panoramic x-rays will then be taken to enable the dentist to plan the apicoectomy, which will be performed under local anesthesia.
The dentist will make a small incision in the gum and expose the root by lifting away the gum. In some cases, a tiny fraction of the jawbone may be removed to properly expose the root. The edge of the root tip and any infected connective tissue will be removed using ultrasonic instruments. The root will be sealed using a retrofill (filling material) and the dentist will suture the gum with several stitches.
This surgery does not require an overnight stay, and full aftercare instructions and pain medications will be provided as needed. After several days, the dentist will remove the stitches, and the connective tissues will fully heal several months after the procedure.
Removal of Dental cysts


A cyst is lined with a kind of tissue called epithelium. This type of tissue normally is found in surface layers, such as the skin and the lining of the mouth. Cysts may form when epithelium cells move into deeper body layers and begin to multiply.
Oral cysts can be found in the jawbone, or in soft tissues such as the salivary glands, skin or inside the mouth.
A cyst is not cancerous but can damage your soft tissue. As the cyst develops, the bone structure around the tooth will feel an extreme amount of pressure. It could eat away from the bone and weaken it.
An oral surgeon usually does this procedure under local anesthesia. If the cyst is infected, you may be given antibiotics.